Introduction and objective
Gleason grading of prostate cancer (PCa) is essential for treatment strategy and prognosis of individual patients. Multiple studies showed inter-observer variation in grading of prostate needle biopsies, but grading variation between pathology laboratories has not yet been examined. Our objective is to analyze grading variation between laboratories and between pathologists within laboratories.
Methods
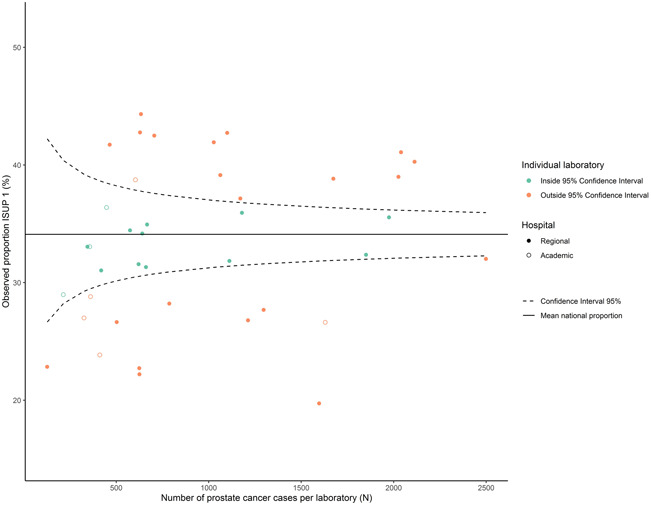
A large population-based observational study was executed among men who were diagnosed with PCa in prostate needle biopsies between January 2017 and December 2019 in the Netherlands. Synoptic (n=12,954) and narrative (n=25,258) pathology reports were retrieved from the nationwide Dutch Pathology registry (PALGA). Primary outcome was the absolute difference in laboratory-specific proportions of International Society of Urological Pathologists (ISUP) grade classes, compared to the national mean and a reference laboratory. Secondary outcome measure was the inter-pathologist variation in ISUP grade within 18 laboratories that agreed on individual analysis. With a multivariate logistic regression of the synoptic reports, we corrected for case-mix factors, including age, number of biopsies and positive biopsies. A laboratory-specific unadjusted odds ratio (OR) was determined for ISUP Grade 1 versus ISUP 2 or higher.
Results
In total, 38,321 reports of 35,258 patients were included. ISUP 1 was assigned to 34.1% of patients, ranging from 19.7 to 44.3% in individual laboratories. Compared to the reference laboratory, 22 labs out of 40 laboratories showed a significantly deviant OR. Laboratory-specific OR ranged from 0.48 (95% confidence interval (CI) 0.39–0.59) to 1.54 (95%-CI 1.22–1.93). Case-mix correction in synoptic reports led to a median difference between the adjusted and the unadjusted laboratory-specific proportion of +0.2%, ranging from -6.8% to +4.0% (Q1;Q3 = -0.9%;+1.8%). Within 13/18 (72.2%) laboratories, significant inter-pathologist variation existed.
Conclusions
Substantial interlaboratory variation in PCa grading was observed between and within Dutch pathology laboratories. Case-mix played a minor role in the observed variation. Better standardization of PCa grading is needed to optimize and harmonize treatment.