Introduction and objective
Multiparametric MRI (mp-MRI) has demonstrated high diagnostic accuracy for clinically signicant PCa (csPCa). However, there is still a substantial variability in mp-MRI protocols and inter-readers’ agreement. We aimed to assess the effect of a central mp-MRI images review on the detection of clinically signicant PCa (csPCa) at a single, tertiary referral centre.
Methods
We relied on a cohort of 319 consecutive men with a positive mp-MRI (PI-RADS≥3) who underwent a targeted biopsy (TBx) and a concomitant systematic biopsy at a single tertiary referral centre between 2017 and 2020. All mp-MRIs were externally performed at different centers. Of those mp-MRIs, 22% (n=77) were centrally reviewed at our centre by a single experienced radiologist. The study outcome was to compare the detection rate of csPCa between the two groups (no-central review [group 1] vs central review [group2]). Furthermore, we compared the distribution of PI-RADS score across the two groups. Multivariable logistic regression analysis (MVA) was used to assess the relationship between mpMRI central review and the detection of csPCa at TBx, after accounting for the following confounders: PSA, prostate volume, PI-RADS (<4 vs ≥4) and biopsy history (biopsy naïve vs repeat biopsy vs active surveillance).
Results
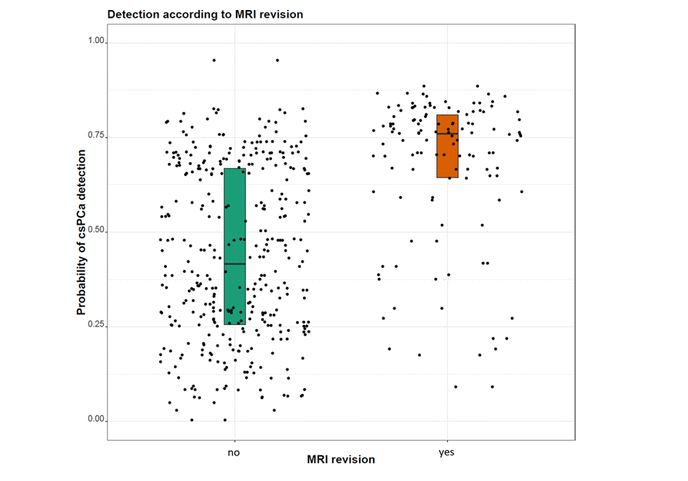
The prevalence of PI-RADS 3, 4 and 5 was 45%, 44% and 11% in group 1 vs 15%, 58% and 27% in group 2 (p<0.01). After central mp-MRI review, PI-RADS was increased, decreased and unchanged in 8%, 39% and 54% of patients, respectively. Overall, csPCa detection at TBx was 46% (n=147). The detection of csPCa in Group 1 vs Group 2 was 41% (n=102) vs 63% (n=45), respectively (p=0.0015, Figure 1). At MVA, PI-RADS (odds ratio[OR]: 4.7), prostate volume (OR: 0.97) and mpMRI central review (OR: 1.6) were signicantly associated with csPCa detection at TBx (all p <0.02). Figure 1 shows the distribution of csPCa detection at TBx between group 1 and 2, showing a statistically signicant difference (p=0.003).
Conclusions
We demonstrated that a central review of mpMRI performed by an experienced radiologist is associated with signicant changes in PIRADS and higher rates of csPCa detection at TBx. Thus, in order to maximize the diagnostic abilities of TBx, a central mpMRI images review is recommended.
Figure 1: