Background
Following treatment of prostate cancer with radical prostatectomy (RP), biochemical recurrence (BCR) can be detected with elevated PSA. This may be attributed to either cancer recurrence or retained benign prostatic gland tissue. Options for detecting malignancy after RP currently entail diagnostic imaging and biopsy with transrectal ultrasound (TRUS). TRUS alone has limited accuracy in detecting recurrence in the prostate bed. MRI fusion-guided biopsy (Fbx) may be a more accurate method of detecting post-RP local recurrence. We hypothesize that Fbx for diagnosing benign versus malignant recurrence in the prostate bed is feasible and produces clinically meaningful results.
Methods
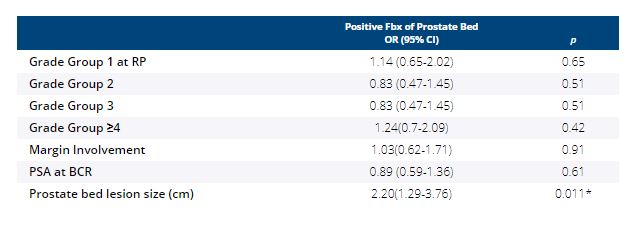
Our institutional database was queried for patients who received RP and demonstrated BCR between February 2015 and July 2020. All patients with evidence of prostate bed recurrence on mpMRI were included in this analysis. Cancer detection via mpMRI-guided fusion biopsy using the UroNav platform was evaluated and patient variables including final Gleason Grade group (GG), margin involvement, PSA at BCR, and prostate bed lesion size were analyzed with univariate logistic regression.
Results
40 patients (median age = 68) with BCR underwent post-RP mpMRI. 25/40 (62.5%) patients had MRI-visible lesions, and among those, 17/25 (68%) patients underwent Fbx of the prostate bed. 15/17 (88.2%) Fbxs detected prostate tissue (either benign or cancer), 11/17 (64.7%) contained cancer, and 4/17 (23.5%) contained benign prostate glands. Median cores per biopsy was 4 (IQR 4-6). Among the 83 cores obtained, 57 (68.6%) cores contained prostate gland tissue and 26 (31.3%) contained fibromuscular tissue. Of those 57 with gland tissue, 33 (57.9%) cores contained cancer, and 24 (42.1%) contained benign prostate tissue. Among patients with benign biopsies, none had further evidence of metastasis at median follow-up of 13.5 months after Fbx and 182 months after RP. On final RP pathology, 4 patients had GG1 disease, 4 had GG2, 4 had GG3, 2 had GG4, and 3 had GG5. 6/17 (35%) patients had positive RP margins. Median prostate bed lesion size was 1.3 cm (IQR 0.9-1.5). Prostate bed lesion size (cm) was the only variable significantly associated with cancer on Fbx (OR = 2.20, 95% CI:1.29-3.76, p = 0.011).
Conclusions
mpMRI-Fbx is a feasible method for reliably targeting prostate bed lesions. With this technique, we found improved accuracy for biopsy-proven recurrence in the prostate bed. This technique will help direct treatment planning of salvage therapies among patients with detectable PSA post-RP.